|
TITLE OF CASE
|
|
A young girl with
renal failure, a red herring and management uncertainty
|
|
SUMMARY
|
|
An
18-year-old female presented with headache, vomiting, lower abdominal pain,
and reduced urine output for two weeks. Having a very high blood pressure on
presentation, the attending physician thought of differentials like
pheochromocytoma and coarctation of aorta, but they were ruled out later on.
The patient’s renal function kept deteriorating in the meanwhile. The imaging
of her abdomen suggested ovarian cyst to be a likely cause of lower abdominal
pain. Ectopic pregnancy and septic abortion were ruled out earlier as well. Without
a proper diagnosis, the patient’s renal function worsened, only to be
salvaged by haemodialysis. In the midst of this red herring, cause of her
renal failure came out to be Zinc Phosphide that the patient had ingested for
suicide. This was only possible because of a repeatedly rigorous history by
the physician underlining the importance of good clinical skills even in the
present era of advanced diagnostic techniques.
|
|
BACKGROUND
|
|
In an era of
highly sophisticated diagnostic gadgets, the physicians tend to rely more and
more on test results rather than practising classical medicine. There is no
doubt that the evolution in diagnostic techniques has helped in pin-pointing
a diagnosis, but it creates diagnostic dilemmas from time to time as well;
which underlines the importance of history taking and a proper physical
examination of the patient. The authors came across such a case where
symptoms and the diagnostic tests were a bit misleading. The patient was
suffering from acute renal failure which was progressing into chronic renal
failure and the cause of which was still unknown. But in the end, repeated
and a thorough history taking helped the patient open up and she confessed
taking a minute amount of Zinc Phosphide which was accessible to her vary
easily as a rodenticide at home. That was the catch. No other diagnostic test
could’ve easily detected this etiology of her renal failure, but a proper and
a thorough history taking solved this malady and the patient was salvaged in
time.
|
|
CASE PRESENTATION
|
|
An 18-year-old Indian female presented
to the Out-Patient Department (OPD) of a tertiary-care teaching hospital with
complaints of headache, nausea and vomiting, lower abdominal pain, puffy face,
and reduced urine output for two weeks. The headache was severe in intensity,
bilateral, non-throbbing, continuous, and without aura. There were two to
three episodes of vomiting which were preceded by nausea, non-projectile in
nature, containing mostly food particles, and not associated with diarrhoea. Her
lower abdominal pain was mild to moderate in intensity, dull in nature, and
non-radiating.
There was no past history of similar
illness, previous hospitalization or any other major illness. There was no
history of similar illness in her family as well. The patient had decreased
appetite since the onset of current illness. Her food habits were otherwise
normal, with unaltered bowel movements and sleep patterns. The patient did
not have any habits pertaining to alcohol and smoking.
The patient had regular menstrual
periods every 28-30 days, lasting for 3-5 days. There was no history of prior
pregnancy or abortion. However, the patient had regular sexual contact and
had missed a menstrual period one month before presenting to the hospital. On
missing a menstrual period, the patient had taken four tablets of i-pill,
which contains levonorgestrel 1.5 mg in a single tablet.
On examination, the patient’s oral
temperature was 98.4° F, pulse rate was 82 per minute, blood pressure was
200/120 mm of Hg, and respiratory rate was 20 per minute. There was
significant pallor in tongue, nailbed, and conjunctiva. There was no evidence
of icterus, clubbing, cyanosis, or oedema.
On
admission, her blood samples were sent for further investigations. The
initial reports were suggestive of acute renal failure (ARF). For a detailed
assessment, ultrasonography (USG) of abdomen and pelvis was carried out. And
to confirm the USG findings, Magnetic Resonance Imaging (MRI) of abdomen was
carried out as well.
|
|
INVESTIGATIONS
|
|
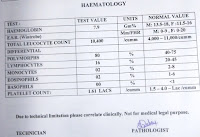
The patient’s reduced urine output
prompted quick investigations. Initially, her Serum Urea and Serum Creatinine
values were 124 mg/dl and 8.9 mg/dl respectively, with haemoglobin 6.6 gm%.
Urine routine microscopy (RM) showed significant albuminuria with pus cells,
some RBCs, some WBCs, but no casts. The similar tests were carried out to
observe the prognosis, but her renal function worsened progressively.
Within next 10 days, her Serum Creatinine
rose to 11.2 mg/dl and Serum Urea was 199 mg/dl. There was sustained
albuminuria along with protein to creatinine ratio in urine was 0.4. During
the disease progression, the patient also developed tachycardia and raised
Jugular Venous Pressure (JVP). The electrocardiogram findings along with the
clinical findings were suggestive of uremic pericarditis.
USG was suggestive of normal renal
size, loss of corticomedullary junction differentiation in both the kidneys,
a right ovarian mass with free fluid in the peritoneal cavity. On MRI, the
ovarian mass turned out to be a cyst which seemed unlikely to cause ARF.
Renal biopsy was planned, but the patient refused. The cause of ARF was still
unclear.
|
|
DIFFERENTIAL
DIAGNOSIS
|
|
·
Pheochromocytoma
·
Coarctation of Aorta
·
Septic Abortion
·
Ruptured ectopic pregnancy
The patient’s high blood pressure at
an age of 18 years made the authors suspicious of either pheochromocytoma or
the coarctation of aorta. But the blood pressure was the same in both arms as
well as lower limbs, and the increase in blood pressure wasn’t episodic.
Hence, both these differentials were ruled out. Besides, the history of
regular sexual contact prompted the authors to think about septic abortion
complicated by renal failure, or a ruptured ectopic pregnancy. The patient
had given the history of taking four i-pill tablets on missing a menstrual
period. But she denied any attempt to have abortion and the Urine Pregnancy
Test (UPT) was negative as well. Thus, these both differentials were off the
table.
|
|
TREATMENT
|
|
Due to
her significantly high blood pressure, the patient was started on Furosemide
and Amlodipine. Ondansetron was started for vomiting, which was later
switched to promethazine. For headache, paracetamol tablet was initially
started, but tramadol was added on the next day, as paracetamol alone was
unable to relieve her severe headache.
The patient’s renal function kept
deteriorating after being admitted to the hospital, as no pin-point diagnosis
was yet to be established. Four sessions of haemodialysis were carried out
over a period of ten days with a view to preventing further deterioration.
|
|
OUTCOME AND
FOLLOW-UP
|
|
The initial Renal Function Test (RFT)
and a significantly low amount of Haemoglobin pointed towards a chronic
problem. But the acute presentation and absence of any such episode
complicated the picture. Besides, based on the USG findings, the authors
suspected that the ovarian mass could be the reason behind the patient’s ARF.
But the patient kept deteriorating before further step could be taken. After
four sessions of Haemodialysis, the patient was stabilised. On stabilisation,
MRI was carried out which was suggestive of ovarian cyst. However, that
ovarian cyst was not causing any obstruction in the urinary tract. So, the authors
were sent back to ground zero. Even after 20-25 days of investigations, there
was no diagnosis. The history was taken again. The patient was taken into
confidence and finally she confessed of ingesting a minute amount of
rodenticide which contained Zinc Phosphide, with a view to committing suicide
on fearing pregnancy.
She was started on intravenous saline
once her RFT touched the base and started recovering well with a normal urine
output. After a few days of observation, she was discharged on request and
was called for a weekly follow-up.
On follow-up, she was found to have
reduced urine albumin, normal blood pressure, and normal urine output. She is
symptomatically better, but her renal progression is still under evaluation.
|
|
DISCUSSION
|
|
When there is a pathology involving a
specific organ, it can be readily diagnosed by imaging techniques and/or
microscopy. But in some cases, the diagnostic techniques fail to answer all
the questions. At that time, the physicians need to take a step back and
reassess the situation to find the answers. This case made the authors
realise that history taking and clinical examination are of utmost importance
when it comes down to assessing the remote possibilities of diagnoses and all
other diagnostic techniques fail to reach a diagnosis.
Zinc Phosphide has been used widely as
a rodenticide. Upon ingestion, it gets converted to phosphine gas in the
body, which is subsequently absorbed into the bloodstream. [1] Phosphine
inhibits cytochrome c oxidase which causes a severe drop in cellular
respiration. There is usually a short interval between ingestion of
phosphides and the appearance of systemic toxicity. Along with impaired
myocardial contractility and pulmonary oedema, metabolic acidosis,
disseminated intravascular coagulation (DIC), and acute renal failure are
frequent. [2] Even though it causes a significant amount of
morbidity and mortality in developing countries, it is widely and easily
available in India as rodenticide, and used by young and productive members
of the society for suicide attempts. [1,3] Sadly, there is neither
a specific diagnostic test, nor an antidote to phosphine; supportive measures
are all that can be offered and should be implemented as required, as the
mortality rate ranges from 37% to 100%. [1,2]
In this case, the patient had ingested
a very minute amount of Zinc Phosphide. Hence, the patient did not have
manifestations of sever systemic involvement, except the renal failure and
gastrointestinal disturbances. The renal failure is generally attributed to
the renal tubular injury which causes anuria or decreased urine output. [4]
Because of such isolated manifestation and absence of an easily accessible
diagnostic modality, the authors were unable to pin-point the diagnose which
hindered the management.
Besides, the history of missed
menstrual period, and an ovarian mass on USG made the clinical picture more
and more complex. It was the patient’s repeated history that directly led to
the diagnosis of renal failure. Thus, the abstract of this case is that as a
physician, one should always keep in mind that the patient is at the centre
of healthcare and a good knowledge of clinical skills never disappoints even
when everything else fails.
|
|
LEARNING
POINTS/TAKE HOME MESSAGES
|
|
1. Zinc
Phosphide is a widely available rodenticide which is commonly used for
suicide in developing countries. It has no antidote; only supportive measures
are all that can be offered to the patient.
2. In
cases where the patient presents with several complaints involving multiple
organ systems, it is possible that the reason behind these complaints are
multiple and totally unrelated, as seen in this case report.
3. When
the symptoms of a patient cannot be described by the available diagnostic
modalities, it is generally fruitful to go through the patient’s history and
clinical examination all over again and see what one might have missed
earlier.
|

























No comments:
Post a Comment